|
Neuro Acupuncture and Ancestral Formula Chinese Herbal Medicine |
|
|
|
|
|
|
|
|
|
|
 |
 |
| WHAT CAUSES CP CEREBRAL PALSY?
|
CP Cerebral Palsy- Its difficult to know the cause of most cases of cerebral palsy, but many have been to 'Black or Red palaces means celebrations, temples, grant events or funeral during their pregnancy according to all the datas of the parents between 75%.There are a lot of data that show that during pregnancy the mother has had some form of bad or horrified experience, or have had been to some kind of ceremony of the unpresent once, where there have many people in an enclose area and that causes shortage of oxygen, recorded to many of CP Cerebral Palsy cases. Others have had bad delivery experience or been expose to high chemicals or eletronic. |
|
CP Cerebral Palsy-Still we are unable to identify exactly, we are unable to determine what caused CP Cerebral Palsy in most children who have congenital CP Cerebral Palsy. We do know that the child who is at highest risk for developing CP Cerebral Palsy is the premature, very small baby who does not cry in the first five minutes after delivery, who needs to be on a ventilator for over four weeks, and who has bleeding in his brain. Babies who have congenital malformations in systems such as the heart, kidneys, or spine are also more likely to develop CP Cerebral Palsy, probably because they also have malformations in the brain.
Seizures in a newborn also increase the risk of CP Cerebral Palsy. There is no combination of factors which always results in an abnormally functioning individual. Even the small premature infant has a better than 90 percent chance of not having CP Cerebral Palsy. There are a surprising number of babies who have very stormy courses in the newborn period and go on to do very well.
In contrast, some infants who have rather benign beginnings are eventually found to have severe mental retardation or learning disabilities.
|
| |
| CP CEREBRAL PALSY - IN THE NEWBORN |
Children with CP Cerebral Palsy have a congenital malformation of the brain, meaning that the malformation existed at birth and was not caused by factors occurring during the birthing process. Not all of these malformations can be seen by the physician, even with today's most sophisticated scans, but when CP Cerebral Palsy is recognized in a newborn, a congenital malformation is suspected. When a diagnosis of CP Cerebral Palsy is made, the mother and father often feel guilty and wonder what they did to cause their child to have this disorder. While it is certainly true that good prenatal care is an essential part of preventing congenital problems, it must be stated that congenital problems, or "birth defects, often occur even when the mother has strictly followed her physician's advice in caring for herself and the developing infant. Though the causes of birth defects are usually unknown, we do know that the developing brain can be affected by several factors. When the fetus is exposed to certain chemicals or infections through the expectant mother, for example. The developing brain can be injured if the expectant mother suffers severe physical trauma or been to special places that give sudden trauma, the fetal brain can be injured, too, but this is rare.
Finally, prematurely and a low birth weight have been shown to be related to an increased incidence of specific disorders. Many chemicals are known to adversely affect the developing brain, alcohol being the most commonly used. The term Fetal Alcohol Syndrome describes the long-term, multi-system effect of alcohol on a child whose mother abused alcohol during the pregnancy. When a fetus is exposed to large amounts of alcohol, several body systems, including the neurological system will almost certainly suffer damage.
Cigarette smoking by the mother has been shown to decrease birth weight, and low birth weight is associated with several disorders, including CP Cerebral Palsy. Severe malnutrition in the mother can adversely affect brain growth in the fetus, and it, too, can result in a low birth weight.
The use of cocaine or crack by the expectant mother is associated with blood vessel complications, and these complications affect many organs as well as the central nervous system. Cocaine use is increasing and thus becoming more prevalent as cause of brain damage in infants. Most infants whose mothers used cocaine during pregnancy develop mental retardation rather than CP Cerebral Palsy, however. Infections such as rubella (German measles), toxoplasmosis, and cytomegalovirus (CMV), ( if a woman has them during pregnancy), also may injure the brain of the fetus. Rubella can be prevented by immunization, prior to becoming pregnant, and the chances of becoming infected with toxoplasmosis can be minimized by not handling the feces of cats and by avoiding raw or uncooked meat.
Congenital infection with human immunodeficiency virus (HIV, the virus that causes AIDS) also causes brain damage in children, though it usually causes mental retardation rather than CP Cerebral Palsy. It is likely that many other infections in the expectant mother injure the developing fetus, but they are not recognized as causative factors because the woman who has the infection either does not recognize the symptoms of infection or is symptom-free. Premature infants are at a much higher risk for developing CP Cerebral Palsy than full-term babies, and the risk increases as the birth weight decreases. Between 5 and 8 percent of infants weighing less than 1500 grams (3 pounds) at birth develop CP Cerebral Palsy, and infants weighing less than 1500 grams are 25 times more likely to develop CP Cerebral Palsy than infants who are born at full term weighing more than 2500 grams. Any premature infants suffer bleeding within the brain, called intraventricular hemorrhages, intracranial hemorrhages. Again, the highest frequency of hemorrhages is found in the babies with the lowest weight: the problem is rare in babies who weigh more than 2000 grams (4 pounds). This bleeding may damage the part of the brain that controls motor function and thereby lead to CP Cerebral Palsy. If the hemorrhage results in destruction of normal brain tissue (a condition called per ventricular leukomalacia) and small cysts around the ventricles and in the motor region of the brain, then that infant is more likely to have CP Cerebral Palsy than an infant with hemorrhages alone.
|
| |
| CP CEREBRAL PALSY BEGINS |
CP Cerebral Palsy:- In the beginning of live, the child is completely dependent on others for his or her safety and protection. Protecting the child from injury is one of the most important responsibilities of the child's parents. One such injury is asphyxia, which can damage the brain in a variety of ways, and is the number one cause of CP Cerebral Palsy in this age group. The three most common causes of asphyxia in the young child are: choking on foreign objects such as toys and pieces of food (including peanuts, popcorn, and hot dogs); poisoning; and near drowning. The brain may also be damaged when it is physically traumatized as a result of a blow to the head. A child who falls or is involved in a motor vehicle accident or is the victim of physical abuse may suffer irreparable injury to the brain.
One form of child abuse is the shaken baby syndrome, in which the caretaker is trying to quiet the baby by shaking too vigorously, causing the brain to strike repeatedly against the skull under high pressure.
Severe infections, especially meningitis or encephalitis, can also lead to brain damage in this age group. Meningitis is inflammation of the meanings ( the covering of the brain and the spinal cord), usually caused by a bacterial infection, and encephalitis is brain inflammation which may be caused by bacterial or viral infections. Either of these infections can cause disabilities ranging from hearing loss to CP Cerebral Palsy to severe retardation.
|
| |
| RESEMBLE CP CEREBRAL PALSY BUT IS NOT IT |
Special kids have many problems in common, especially problems involving interactions with family members and society at large. The physical and medical problems of children with disabilities vary widely, however. Some of the problems caused by various disorders resemble those affecting children with CP Cerebral Palsy, but on closer inspection the medical issues turn out to be quite distinct.
CP Cerebral Palsy from medical over dose or wrong chemicals, because these injuries can occur at any age and the severity of the problems caused by these brain injuries changes over time. We can also say that disorders that are primarily of muscle, nerve, and bone are not CP Cerebral Palsy by definition. Such conditions include muscular dystrophy, peripheral neuropathies such as Charcot-Marie- Tooth disease, and osteogenesis imperfect.
All of these conditions are associated with specific medical problems. Children with progressive neurologic disorders (including Rett's syndrome, leukodystrophy, and Tay-Sach's disease) also have medical needs which are different from those of children with CP Cerebral Palsy.
Some children with chromosomal anomalies (for example, trisomy 13 and 18) or congenital disorders (hereditary spastic paraplegia, for example) may appear similar to children with CP Cerebral Palsy; others, such as children with Down's syndrome, appear very different from children with CP Cerebral Palsy. Children with these disorders have some problems in common with children who have CP Cerebral Palsy; they also have problems that are unique for children with that specific disorder.
|
| |
| DIAGNOSIS OF CP CEREBRAL PALSY |
CP Cerebral Palsy :-Most normal kids should recognise toys at 3-4 months, sitting at 6-7 months, walk at 10-14 months, are based on motor function. A physician may suspect CP Cerebral Palsy in a child whose development of these skills is delayed. In making a diagnosis of CP Cerebral Palsy, the physician takes into account the delay in developmental milestones as well as physical findings that might include abnormal muscle tone, abnormal movements, abnormal reflexes and persistent infantile reflexes.
Making a definite diagnosis of CP Cerebral Palsy is not always easy, especially before the child's first birthday. In fact, diagnosing CP Cerebral Palsy usually involves a period of waiting for the definite and permanent appearance of specific motor problems.
Most children with CP Cerebral Palsy can be diagnosed by the age of 18 months, but eighteen months is a long time for parents to wait for a diagnosis, and this is understandably a difficult period for them. Making a diagnosis of CP Cerebral Palsy is also difficult when, for example, a two-year- old has suffered a head injury. The child may immediately appear to be severely injured, and three months after the injury he may have symptoms that are typical of a child with CP Cerebral Palsy. But one year after the injury such a child may be completely normal. This child does not have CP Cerebral Palsy. Although he has a scar on his brain, the scar is not permanently impairing his motor activities. After injury, waiting and observing are necessary before the diagnosis can be made.
Diagnosis of CP Cerebral Palsy, examination is the physical evidence of abnormal motor function. A diagnosis of CP Cerebral Palsy cannot be made on the basis of blood test, though the physician may order such tests to exclude other neurologic diseases (such as those mentioned above).
Blood tests and chromosome analysis are helpful in diagnosing hereditary conditions that may influence the parents' future child-bearing decisions. When the tests indicate that a child's condition is something other than CP Cerebral Palsy and that the condition is inherited, family members will benefit from genetic counseling. CP Cerebral Palsy is not a hereditary condition, however, and these tests will neither establish nor rule out a diagnosis of CP Cerebral Palsy.
Magnetic resonance imaging (MRI) and Computed Topography (CT) scans are often ordered when the physician suspects that the child has CP Cerebral Palsy. These tests may provide evidence of hydrocephalus (an abnormal accumulation of fluid in the cerebral ventricles), and they may be used to exclude other causes of motor problems.
Cerebral Palsy- CP -These scans do not prove whether a child has a CP Cerebral Palsy; nor do they predict how a specific child will function as she grows. Thus, children with normal scans may have severe CP Cerebral Palsy, and children with clearly abnormal scans occasionally appear totally normal or have only mild physical evidence of CP Cerebral Palsy. As a group, though, children with CP Cerebral Palsy do have brain scars, cysts, and other changes which show up on scans more frequently than in normal children. Therefore, when a scar is seen on a CT scan of the brain of a child whose physical examination suggests he may have CP Cerebral Palsy, the scar is one more piece of evidence indicating that the child is likely to have motor problems in the future.
CP Cerebral Palsy may be classified by the type of movement problem (such as spastic or athetoid CP Cerebral Palsy) or by the body parts involved (hemiplegia, diplegia, and quadriplegia). Spasticity refers to the inability of a muscle to relax, while athetosis refers to an inability to control the movement of a muscle.
CP Cerebral Palsy- Infants who at first are hypo tonic wherein they are very floppy may later develop spasticity. Hemiplegia is CP Cerebral Palsy that involves one arm and one leg on the same side of the body, whereas with diplegia the primary involvement is both legs. Quadriplegia refers to a pattern involving all four extremities as well as trunk and neck muscles. Another frequently used classification is ataxia, which refers to balance and coordination problems.
CP Cerebral Palsy-The motor disability of a child with CP Cerebral Palsy varies greatly from one child to another; thus generalizations about children with CP Cerebral Palsy can only have meaning within the context of the subgroups described above. For this reason, subgroups will be used in this book whenever treatment and outcome expectations are discussed. Most professionals who care for children with CP Cerebral Palsy understand these diagnoses and use them to communicate about a child's condition.
CP Cerebral Palsy-A useful method for making subdivisions is determined by which parts of the body are involved. Although almost all children with CP Cerebral Palsy can be classified as having hemiplegia, diplegia, or quadriplegia, there are significant overlaps which have led to the use of additional terms, some of which are very confusing. To avoid confusion, most of the discussion in his book will be limited to the use of these three terms. Occasionally such terms as paraplegia, double hemiplegia, triplegia, and pentaplegia may occasionally be encountered by the reader; these classifications are also based on the parts of the body involved. The dominant type of movement or muscle coordination problem is the other method by which children are subdivided and classified to assist in communicating about the problems of CP Cerebral Palsy.
The component which seems to be causing the most problem is often used as the categorizing term. For example, the child with spastic diplegia has mostly spastic muscle problems, and most of the involvement is in the legs, but the child may also have a smaller component of athetosis and balance problems. The child with athetoid quadriplegia, on the other hand, would have involvement of both arms and legs, primarily with athetoid muscle problems, but such a child often has some ataxia and spasticity as well. Generally a child with quadriplegia is a child who is not walking independently.
The reader may be familiar with other terms used to define specific problems of movement or muscle function terms such as: dystonia, tremor, ballismus, and rigidity.
The words severe, moderate, and mild are also often used in combination with both anatomic and motor function classification terms (severe spastic diplegia, for example), but these qualifying words do not have any specific meaning.
|
| |
| WHAT IS CP Cerebral Palsy? |
Usually asked by parents after they are told their child has CP Cerebral Palsy are .What will my child be like and -Will he walk. Predicting what a young child with CP Cerebral Palsy will be like or what he will or will not do (called the prognosis) is very difficult. Any predictions for an infant under six months of age are little better than guesses, and even for children younger than one year it is often very difficult to predict the pattern of involvement. By the time the child is two years old, however, the physician can determine whether the child has hemiplegia, diplegia, or quadriplegia.
Based on this involvement pattern, some predictions can be made. It is worth saying again that children with CP Cerebral Palsy do not stop doing activities once they have begun to do them. Such a loss of skills, called regression, is not characteristic of CP Cerebral Palsy. If regression occurs, it is necessary to look for a different cause of the child's problems. In order for a child to be able to walk, some major events in motor control have to occur. A child must be able to hold up his head before he can sit up on his own, and he must be able to sit independently before he can walk on his own. It is generally assumed that if a child is not sitting up by himself by age 4 or walking by age 8, he will never be an independent walker. But a child who starts to walk at age 3 will certainly continue to walk and will be walking when he is 13 years old unless he has a disorder other than CP Cerebral Palsy.
Difficulty to make early predictions of speaking ability or mental ability than it is to predict motor function. Here evaluation is much more reliable after age 2, although a motor disability can make the evaluation of intellectual function quite difficult.
Sometimes "motor-free" tests which can assess intellectual ability without, the person being tested, needing to use his hands are administered by psychologists who have expertise in their use. Overall, the intellectual ability of the person, far more than their physical disability, will determine the person's prognosis. In other words, mental retardation is far more likely than CP Cerebral Palsy to impair a child's ability to function.
|
| |
| CP Cerebral Palsy - EARLY STAGE |
Parents are naturally concerned when their newborn child has problems, and physicians need to evaluate the child's condition and prognosis as well as they can. For example, evidence of a bleed in the child's brain should be discussed with parents, although the outcome of such a bleed cannot be predicted.
The diagnosis of CP Cerebral Palsy cannot be made at birth and, most assuredly, the extent and severity of involvement that an individual child might eventually have is impossible to assess at birth.
Many neonatologists, aware of the interaction that generally occurs between the newborn and parents, avoid discussing the child's problems in detail because they want to permit this interaction to take place. The presumption of a bleak future for a child sometimes causes parents to withdraw from the child and this can have a significant negative effect on the child. Physicians usually communicate their concerns in terms of the child's symptoms, such as muscle problems, and prepare parents for the possibility of neurologic damage. Clearly, it is part of the physician's role to inform parents, but the variability of outcome makes it virtually impossible for the physician to predict the future, and so the physician must weigh the need to inform (and the imprecision of information) against the need for the parents to have hope for, and to become close to their child.
|
| |
| CP Cerebral Palsy and RESEARCH |
CP Cerebral Palsy - Many times when a child is a few years old and severely disabled, parents begin to wonder whether treatment should have been less aggressive than it was. Given the tremendous uncertainties in outcome, physicians and parents usually choose to treat newborns and preserve life with the hope that the outcome will be a good one. |
| |
Please feel free to contact or email us for further details at : |
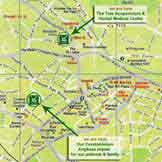
THE TOLE ACUPUNCTURE - HERBAL MEDICAL CENTRE SDN BHD.
Lot 2.01, 2nd Floor,
Medical Specialist Floor,
Menara KH (Menara Promet),
Jalan Sultan Ismail, 50250 Kuala Lumpur.
Malaysia
Tel No : +603-21418370 / +603-21451671
Whatsapp (only): +6012-7688284
Acupuncture Time : |
| Operating Hours : |
| Monday : 10AM - 6PM |
| Tuesday : 1PM - 7PM |
| Wednesday to Saturday : 10AM - 7PM |
| Sunday : 12PM - 4PM |
| *(Malaysia Time) |
| |
|
|
|
|
|
 |
Easiest way to reach us, click below! |
|
|
| |
We can send herbs to your home by: |
|
|
| |
We accept the following payment options in our centre. For Online Payment, please use Direct Transfer. |
|
|
| |
The Tole's Opening Ceremony |
Our New Acupuncture Centre was officially open by our Health Minister YAB Dato' Lee Kim Sai on 31st January 1993. |
YAB Dato' Lee Kim Sai and Dato' Leong Hong Tole (D.S.T.M) - [World Known as MasterTole] |
|
|
|
| |
| |
Share us with your friends. |
They may need our assistance! |

LIKE OUR FACEBOOK PAGE! |
| |

FOLLOW OUR TIKTOK PAGE! |
| |

FOLLOW OUR INSTAGRAM PAGE! |
| |
|
| |
The Star News |
|
|
The Star Newspaper report on Our Master's Acupuncture and Herbal TCM on 5th February 2011, Saturday. |
|
|
| |
|
|
 The Tole Officially Opened by our Health Minister. The Tole Officially Opened by our Health Minister.
- Acupuncture Centre
|
|
|
| |
|
Contact Us
Neuro Acupuncture and Herbal Medicine |
THE TOLE
ACUPUNCTURE-HERBAL MEDICAL CENTRE SDN BHD
Lot 2.01, 2nd Floor, Medical Specialist Floor, Menara KH (Menara Promet), Jalan Sultan Ismail, 50250 Kuala Lumpur
Tel: +603-21418370
+603-21451671
Whatsapp (only): +6012-7688284
| Acupuncture Time : |
Operating Hours : |
Mon : 10AM - 6PM |
Tue : 1PM - 7PM |
Wed to Sat : 10AM - 7PM |
Sun : 12PM - 4PM |
*(Malaysia Time) |
| |
* E-mail consultation with Master and Assistant.
Ask by e-mail

|
|
|
| |
Accommodation
Neuro Acupuncture and Herbal Medicine |
|
CONDOMINIUM |
|
| |
|
|
| |
|
| |
|
| |
Easiest way to reach us, click below! |
|
|
| |
|
|